Navigating the complexities of patient discharge can be quite a challenge for both healthcare providers and patients alike. That’s where a well-structured nursing hospital discharge checklist template comes into play, offering a systematic approach to ensure every critical step is covered. It’s more than just a list; it’s a vital tool designed to streamline the process, enhance patient safety, and ultimately make the transition from hospital to home as smooth as possible. For nurses, it provides clarity and consistency, ensuring no detail is overlooked in what can often be a busy and high-stakes environment.
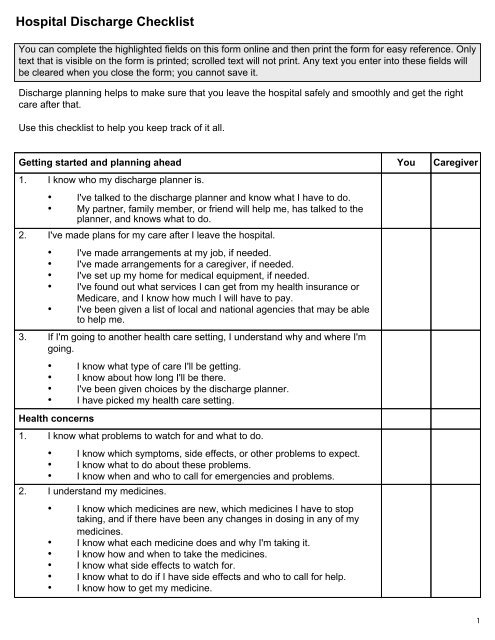
Discharge planning isn’t just about sending a patient home; it’s about preparing them for continued recovery and self-care. Without a clear guide, important information regarding medications, follow-up appointments, wound care, or red flag symptoms can easily be missed. This can lead to confusion, anxiety, and even preventable readmissions, which are costly for healthcare systems and detrimental to patient well-being. A robust checklist acts as a safety net, guaranteeing that all necessary education and resources are provided before the patient walks out the door.
This article will delve into the critical components of an effective discharge checklist, explore why it’s indispensable for modern nursing practice, and offer insights into how to implement and utilize one to its fullest potential. Our aim is to equip nurses and healthcare administrators with the knowledge to optimize their discharge procedures, fostering better patient outcomes and more efficient healthcare operations.
Why a Comprehensive Discharge Checklist is Essential for Patient Safety and Smooth Transitions
The moment a patient is ready to leave the hospital is a pivotal point in their care journey. It signifies a shift from acute, supervised medical attention to self-management or care provided by family members. This transition, if not handled meticulously, can pose significant risks. A comprehensive discharge checklist acts as a blueprint, ensuring that every aspect of the patient’s post-hospital care is addressed, understood, and planned for. It standardizes the process, reducing variability and the potential for human error, which are crucial elements in maintaining high standards of patient safety.
Beyond safety, a well-executed discharge process contributes significantly to patient satisfaction. When patients feel prepared, informed, and supported, their confidence in managing their health at home increases. This positive experience not only improves their physical recovery but also their psychological well-being. Nurses play a central role in this, and a checklist empowers them to deliver consistent, high-quality care even amidst their demanding schedules.
One of the primary benefits is the thoroughness it brings to patient education. Discharge instructions can be overwhelming for patients and their families, especially after a medical event. A checklist ensures that all key topics are covered in a structured manner, from understanding new medications to recognizing warning signs that require medical attention. This systematic approach allows nurses to break down complex information into manageable parts, facilitating better comprehension and retention.
Moreover, a comprehensive checklist aids in medication reconciliation, a critical step to prevent adverse drug events. It ensures that patients leave with the correct medications, dosages, and instructions, cross-referencing against their hospital medication list and any pre-admission prescriptions. This meticulous review helps to avoid dangerous drug interactions or omissions, which are common causes of readmission.
The checklist also serves as a vital communication tool. It ensures that all members of the healthcare team – physicians, nurses, pharmacists, social workers, and case managers – are aligned on the discharge plan. This interdisciplinary collaboration is paramount for a holistic approach to patient care, guaranteeing that every professional contributes their expertise to a seamless transition.
Finally, integrating a detailed discharge checklist helps healthcare facilities meet regulatory requirements and quality benchmarks. It provides documented evidence of thorough discharge planning, which is essential for accreditation and demonstrates a commitment to patient-centered care. By mitigating the risks of readmission, it also contributes to the financial health of the organization, as many healthcare systems face penalties for high readmission rates.
Key Elements to Include in Your Checklist
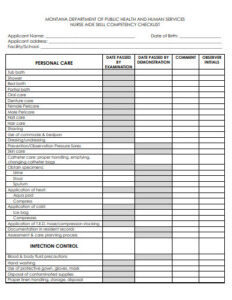
A robust discharge checklist should cover several key areas. This includes patient education on their condition, new or changed medications with dosage and schedule, follow-up appointment details, dietary restrictions, activity limitations, warning signs to watch for, and contact information for questions. It also encompasses logistical elements like transportation arrangements and ensuring all personal belongings are accounted for.
The Role of Nurses in the Discharge Process
Nurses are at the forefront of discharge planning and education. They are often the last healthcare professional a patient interacts with before leaving the hospital. Their role involves assessing the patient’s readiness for discharge, delivering personalized education, coordinating with other team members, and ensuring the patient and their family feel confident and prepared. The nursing hospital discharge checklist template is an invaluable aid in fulfilling these responsibilities efficiently and effectively.
Streamlining the Discharge Process: Tips and Best Practices
Implementing a robust discharge checklist is just the first step; effectively integrating it into daily practice requires thoughtful planning and continuous effort. One best practice is to move towards digital templates where possible. Digital checklists can be easily updated, customized for specific patient populations or units, and integrated with electronic health records (EHRs). This not only improves efficiency but also ensures better documentation and accessibility for all members of the care team. Training staff on how to use the chosen template consistently and effectively is paramount to its success, emphasizing the why behind each item on the list.
Another crucial tip is to involve patients and their families in the discharge planning process as early as possible. This proactive approach allows them to ask questions, understand their roles in continued care, and feel more engaged in their recovery journey. Providing educational materials in clear, accessible language and in various formats (e.g., printed, digital, videos) can further enhance comprehension and adherence to post-discharge instructions.
Regularly review and update your discharge checklist template based on feedback from nurses, patients, and outcomes data. Healthcare is constantly evolving, and your tools should evolve with it. Monitoring readmission rates and patient satisfaction scores can provide valuable insights into areas where the checklist or the discharge process itself might need refinement. This continuous quality improvement cycle ensures that your hospital discharge process remains effective, patient-centered, and aligned with the latest evidence-based practices.
Effective discharge planning is a cornerstone of quality patient care, significantly impacting recovery and preventing complications after a hospital stay. By meticulously preparing patients and their families for the transition home, healthcare providers can foster better health outcomes, reduce the burden of readmissions, and enhance the overall patient experience. It’s an investment in both immediate patient well-being and long-term public health.
The journey from hospital to home is a critical phase that demands careful attention and coordination. By embracing comprehensive discharge protocols and utilizing tools like a standardized checklist, healthcare institutions can empower their nursing staff, improve communication, and ensure that every patient receives the support and information needed for a successful recovery. This dedication to thorough discharge planning ultimately strengthens the entire continuum of care.